9.2 General assessment and management guidelines
See reference 27
9.2.1 General considerations
Chronic misuse of drugs is incompatible with safe vehicle driving. Careful individual assessment must be made of drivers who misuse alcohol or other substances (prescribed or illicit). Substance misuse may not be confined to a single drug class, and people may use multiple substances in combination. In addition, people who misuse substances may change from one substance to another. Occasional use of these drugs also requires very careful assessment. In particular, the health professional should be satisfied that the use of these drugs is not going to affect a commercial vehicle driver in the performance of their duties.
During clinical assessment, patients may understate or deny substance use for fear of consequences of disclosure. The acute and chronic cognitive effects of some substance use also contribute to difficulty in obtaining an accurate history and identification of substance use. Assessment should therefore incorporate a range of indicators of substance use in addition to self-report, including objective assessments. Urine drug screens, oral fluid testing and blood testing provide objective evidence of recent drug use but may only give a limited historical context. Hair testing can provide a longitudinal detection window measured in months through which to assess remission.
Secondary opinion from an appropriate specialist, such as an addiction medicine specialist or addiction psychiatrist, may be necessary. Further assessments and/or objective evidence from biological monitoring (e.g. supervised drug screening) by the treating doctor may be indicated, including relevant investigations, particularly in the case of commercial vehicle drivers. In particular, people with substance use disorder and mental illness, acquired brain injury or chronic pain comorbidities may have a level of complexity requiring specialist assessment. On-road practical driving assessments may assist in some cases to determine fitness to drive.
9.2.2 Alcohol dependence
See reference 28
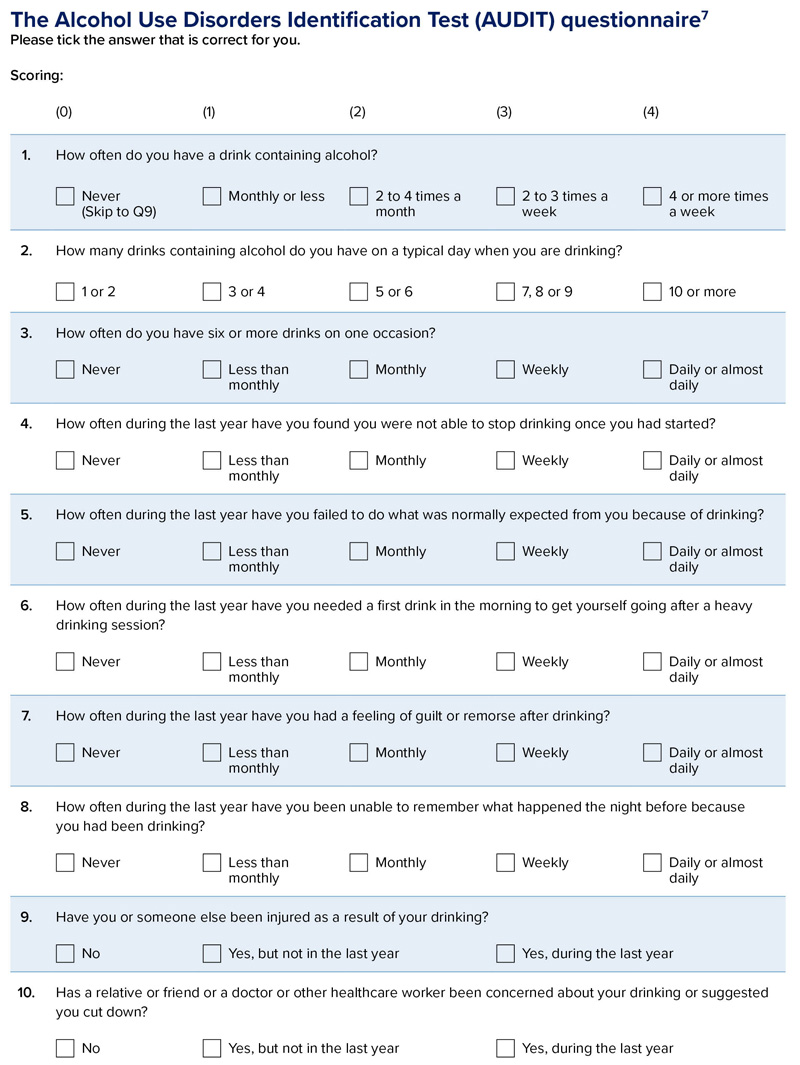
Screening tests may be useful for assessing alcohol dependence and other substance use disorders. For example, the Alcohol Use Disorders Identification Test (AUDIT) may be used to screen for alcohol dependence (refer to Figure 16). The total maximum score is 40. A score of eight or more indicates a strong likelihood of hazardous or harmful alcohol consumption. Referral to an appropriate specialist, such as an addiction medicine specialist or addiction psychiatrist, should be considered, particularly in the case of commercial vehicle drivers. The AUDIT relies on accurate responses to the questionnaire and should be interpreted in the context of a global assessment that includes other clinical evidence. For more information about the AUDIT questionnaire, refer to https://www.who.int/publications/i/item/audit-the-alcohol-use-disorders-identification-test-guidelines-for-use-in-primary-health-care
.
Alcohol ignition interlocks are devices that prevent a car starting if the driver has been drinking. All states and territories have alcohol interlock programs where a driver who has been convicted of specified drink-driving offences is subject to a licence condition that they only drive a motor vehicle with an alcohol interlock fitted. An alcohol interlock condition may be ordered by a court as part of the sentencing or the licence restoration process, or imposed by the driver licensing authority in some circumstances. Interlocks may also be used voluntarily by drivers who are found to have alcohol dependence. A zero BAC condition can be set independently of an interlock condition or continue at the conclusion of an interlock program. Programs vary between the states and territories. For more information see Appendix 5. Alcohol interlock programs.
Figure 16: The Alcohol Use Disorders Identification Test (AUDIT) questionnaire
9.2.3 Opioid dependence
Opioid dependency includes patients taking opioid medication for chronic pain. People on stable doses of opioid analgesics for chronic pain management and people taking buprenorphine or methadone for their opioid dependency may not have a higher risk of a crash than the general population, providing the dose has been stabilised over some weeks and they are not abusing other impairing drugs.
The risk of impairment due to unsanctioned use of opioids or other sedatives is a consideration. Short-acting opioids, particularly parenteral forms, may cause fluctuation in blood levels of opioids, which would be expected to be incompatible with safe driving. People using these agents should be referred for assessment by an appropriate specialist such as an addiction medicine specialist, addiction psychiatrist or pain medicine specialist.
Further guidance on opiate prescribing can be found from:
- the Royal Australian College of Physicians’ Prescription Opioid Policy: Improving management of chronic non-malignant pain and prevention of problems associated with prescription opioid use32
- the Australian and New Zealand College of Anaesthetists and Faculty of Pain Management’s Statement regarding the use of opioid analgesics in patients with chronic non-cancer pain33
- the Royal Australian College of General Practitioners’ Prescribing drugs of dependence in general practice29, 30, 31
- local health agency websites.
9.2.4 Non-cooperation in cessation of driving
Should the person continue to drive despite advice to the contrary, the health professional should consider the risk posed to other road users and take reasonable measures to minimise that risk, including notifying the driver licensing authority. This is particularly relevant for commercial vehicle drivers. Refer to Part A section 3.3.1. Confidentiality, privacy and reporting to the driver licensing authority and Appendix 3.2. Legislation relating to reporting by health professionals. Refer to information about alcohol interlock programs.
